|
HOUSTON
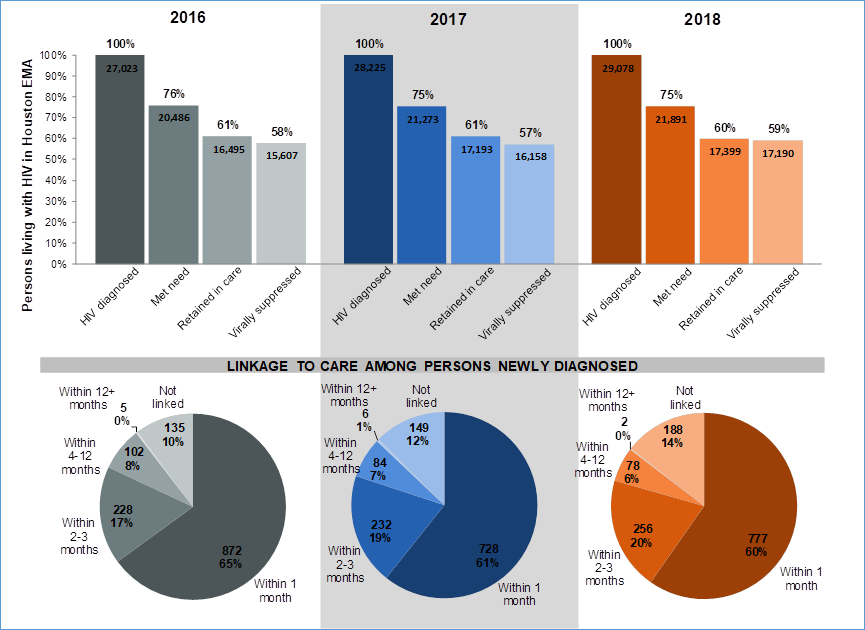
EMA HIV CARE CONTINUUM What is the Care Continuum? The HIV Care Continuum, previously known as a Treatment
Cascade, was first released in 2012 by the Centers for Disease
Control and Prevention (CDC). It represents the sequential stages of HIV
care, from being diagnosed with HIV to suppressing
the HIV virus through treatment. Ideally, the Care Continuum describes a
seamless system of HIV prevention and care services, in which people living
with HIV (PLWH) receive the full benefit of HIV treatment by being diagnosed,
linked to care, retained in care, and taking HIV medications as prescribed to
achieve viral suppression. The Houston Care Continuum (HCC) The HCC is a diagnosis-based continuum. The HCC
reflects the number of PLWH who have been diagnosed ("HIV
diagnosed"); and among the diagnosed, the numbers and proportions of
PLWH with records of engagement in HIV care ("Met Need"), retention
in care ("Retained in Care"), and viral suppression ("Virally
Suppressed") within a calendar year. Although retention in care is a
significant factor for PLWH to achieve viral suppression, ‘Virally
Suppressed’ also includes those PLWH in the Houston EMA whose
most recent viral load test of the calendar year was <200 copies/mL but
who did not have evidence of retention in care. Linking newly diagnosed individuals into HIV medical
care as quickly as possible following initial diagnosis is an essential step
to improved health outcomes. In the HCC, initial linkage to HIV medical care
("Linkage to Care") is presented
separately as the proportion of newly
diagnosed PLWH in the Houston EMA who were successfully linked to medical
care within one month, three months or within one year after diagnosis. Figure 1: Houston
EMA HIV Care Continuum, 2016-2018**
Source: Bureau of
Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention, Houston
Health Department, 2020
From 2016-2018, the total number of persons diagnosed
with HIV increased each year and the percentage of those with met need,
retention, and viral suppression remained relatively constant. ·
The percentage of newly diagnosed PLWH
linked to care within one month of diagnosis decreased from 65% to 60% from
2016 to 2018. Disparities in
Engagement among Key Populations Multiple versions of the HCC have
been created to illustrate engagement disparities and service gaps that
key populations encounter in the Houston EMA. It is important to note that
available data used to construct each version of the Houston HCC do not
portray the need for activities to increase testing, linkage, retention, ART
access, and viral suppression among many other at-risk key populations, such
as those who are intersex, experiencing homelessness, or those recently
released from incarceration. The Houston EMA Care
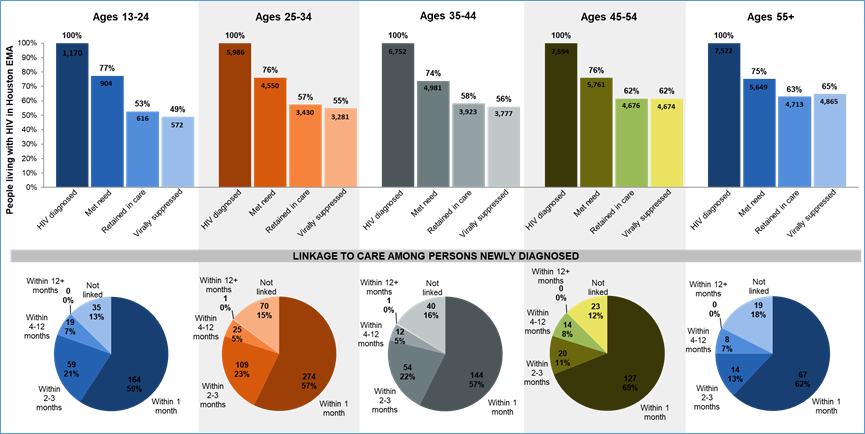
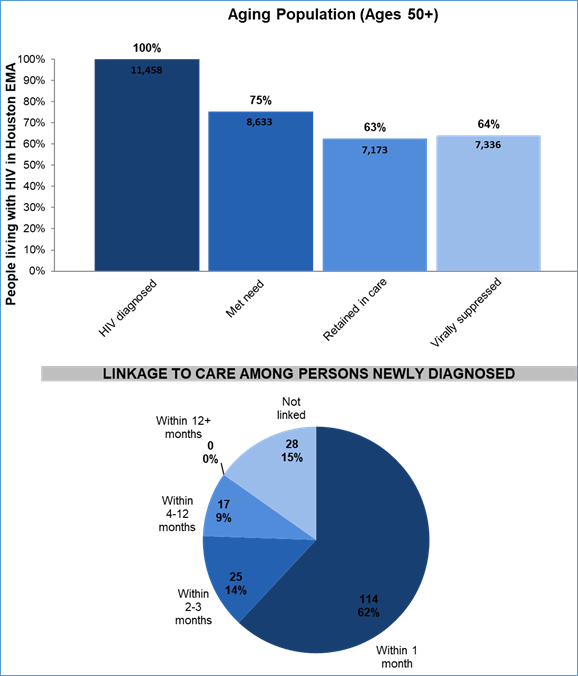
Continuum, by Age Figure 2: Houston
EMA HIV Care Continuum by Age Group, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
Houston Health Department, 2020 Figure 3: Houston
EMA HIV Care Continuum by Age Group, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
Houston Health Department, 2020 ·
Younger adults had lower percentages
of retention and viral suppression compared to older adults. ·
Middle age adults (25-44 years old)
had the lowest proportion of newly diagnosed PLWH who were
linked to care within one month of diagnosis when compared to other
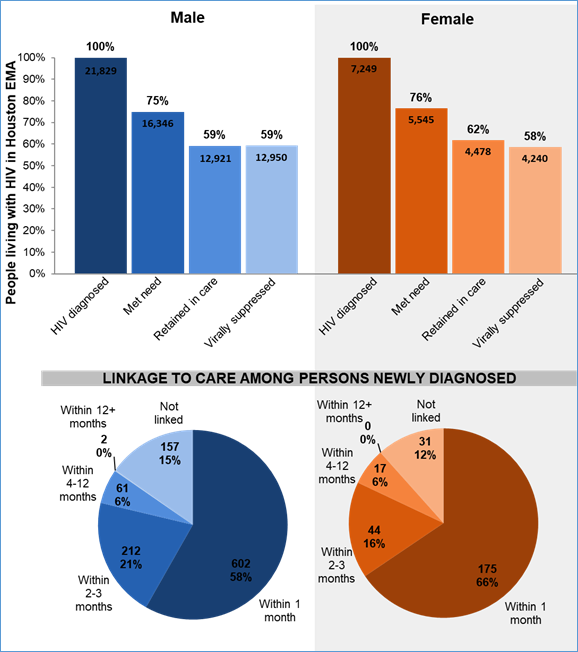
age groups. The Houston EMA Care Continuum, by Sex Assigned at Birth/Current Gender Figure 4: Houston EMA HIV Care
Continuum by Sex Assigned at Birth, 2018**
Source: Bureau of
Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention, Houston
Health Department, 2020 ·
Females living with HIV in the Houston
EMA in 2018 had a slightly higher proportion of individuals with met need and
retention in care than males living with HIV, although females had a slightly
smaller proportion of viral suppression. ·
The proportion of newly diagnosed
females linked to care within the first month after diagnosis was higher than
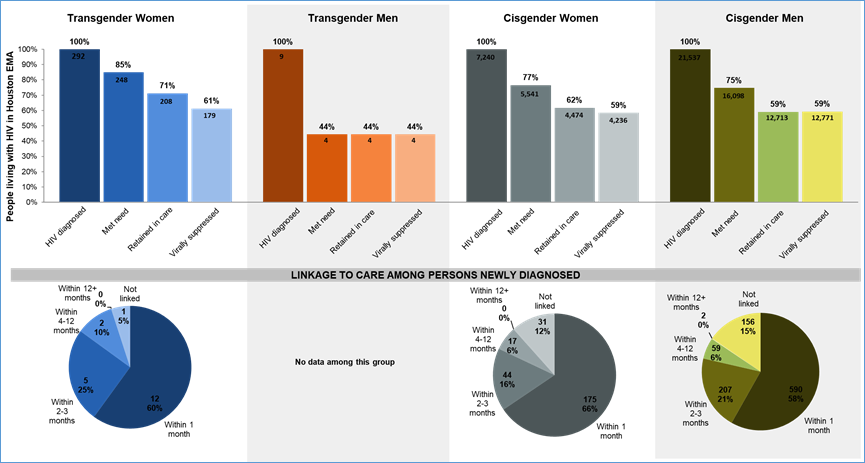
males (66% vs. 58%). Figure 5: Houston EMA HIV Care Continuum
by Current Gender, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
Houston Health Department, 2020 ·
Transgender women living with HIV in
the Houston EMA in 2018 had the highest proportion of individuals with met
need, retention in care, and viral suppression. ·
Transgender men living with HIV in the
Houston EMA in 2018 had the lowest proportion of individuals with met need,
retention in care, and viral suppression. Extreme caution should
be exercised in interpretation, however, due to the very small numbers
of transgender men represented in this data. ·
The proportion of newly diagnosed
people linked to care within the first month after diagnosis was lower for
transgender women compared to cisgender women. However, there
were few transgender individuals represented in the data and
percentages can vary widely with small increases/decreases. The Houston EMA Care Continuum, by Sex Assigned at Birth and
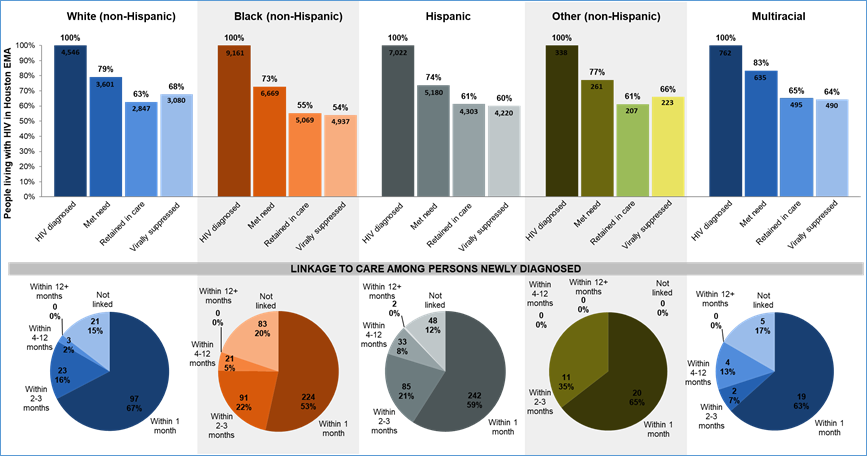
Race/Ethnicity Figure 6: Houston EMA HIV Care
Continuum by Sex Assigned at Birth = Male and Race/Ethnicity, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
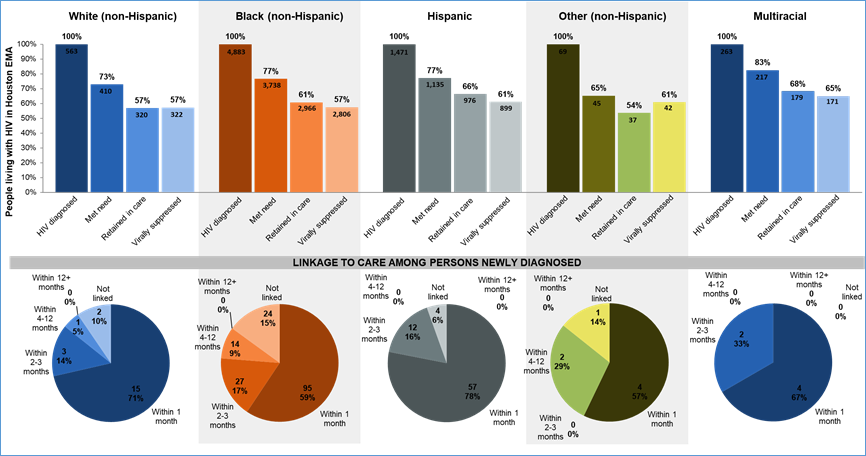
Houston Health Department, 2020 Figure 7: Houston EMA HIV Care Continuum by Sex
Assigned at Birth = Female and Race/Ethnicity, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
Houston Health Department, 2020 ·
Compared to White (non-Hispanic) and
multiracial males, all other males living with HIV had lower proportions of
met need, retention in care, and viral suppression in 2018. ·
Among females, Other
(non-Hispanic) PLWH had the lowest proportion of individuals with evidence of
met need and retention in care while Black and White (non-Hispanic) PLWH had
the lowest proportion of individuals with evidence of viral suppression. ·
Among those newly diagnosed with HIV,
Hispanic females and White (non-Hispanic) males had
the highest proportion linked to care within 1 month of diagnosis. ·
Overall, Other
(non-Hispanic) females living with HIV had the lowest proportion of
individuals with met need across all birth sex and race/ethnicity groups.
However, this group had few individuals and percentages can vary widely with
small increases/decreases. White (non-Hispanic) females and Black
(non-Hispanic) males living with HIV had the next lowest proportion of
individuals with met need. ·
Overall, Other
(non-Hispanic) females living with HIV had the lowest proportion of
individuals retained in care across all birth sex and race/ethnicity groups.
However, this group had few individuals and percentages can vary widely with
small increases/decreases. Black (non-Hispanic) males living with HIV had the
next lowest proportion of individuals retained in care. ·
Overall, Black (non-Hispanic) males
living with HIV had the lowest proportion of individuals virally suppressed
across all birth sex and race/ethnicity groups. White (non-Hispanic) males
living with HIV had the highest proportion of individuals virally suppressed. The Houston EMA Care Continuum, by
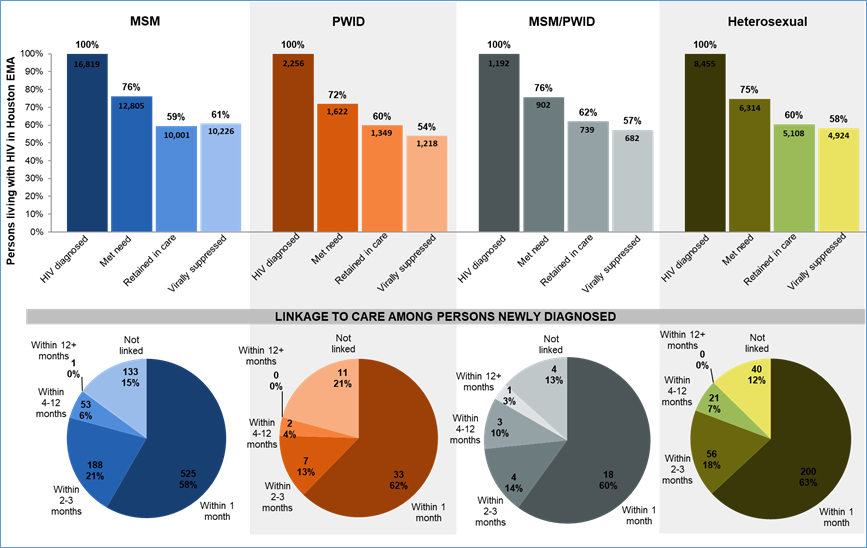
Transmission Risk Factor* *Transmission
risk factors that are associated with increased risk of HIV exposure and
transmission include men who have sex with men (MSM), people who inject drugs
(PWID), MSM who also inject drugs (MSM/PWID), and heterosexual exposure. Figure 8: Houston EMA HIV Care
Continuum by Transmission Risk, 2018**
Source:
Bureau of Epidemiology and Bureau of HIV/STD and Viral Hepatitis Prevention,
Houston Health Department, 2020 ·
Although MSM have a higher number of
PLWH than the other risk groups, the proportion of diagnosed MSM living with
HIV with evidence of met need and retention in care is similar to those
observed for other risk groups. ·
MSM have a higher proportion of
diagnosed PLWH who are virally suppressed but a
lower proportion of newly diagnosed PLWH who were successfully linked to care
within one month of initial diagnosis. Those with a transmission risk factor
of heterosexual contact had the highest proportion of people linked to care
within one month of initial diagnosis. ·
Overall, PWID as a primary
transmission risk factor exhibited the lowest proportions of individuals with
met need and viral suppression. ** 2018 data should be used with caution -- it
may be underrepresented due to unforeseen data importing issues at Texas
DSHS. Updates to 2018 data will occur in the future. Questions
about the Houston EMA HIV Care Continuum can be directed
to the Office of Support: FeedbackRWPC@hctx.net
or call 832-927-7926. |